AHF’s mission is to combat the cascading issues stemming from limited healthcare access.
Limited Healthcare Access: Declining Health Outcomes
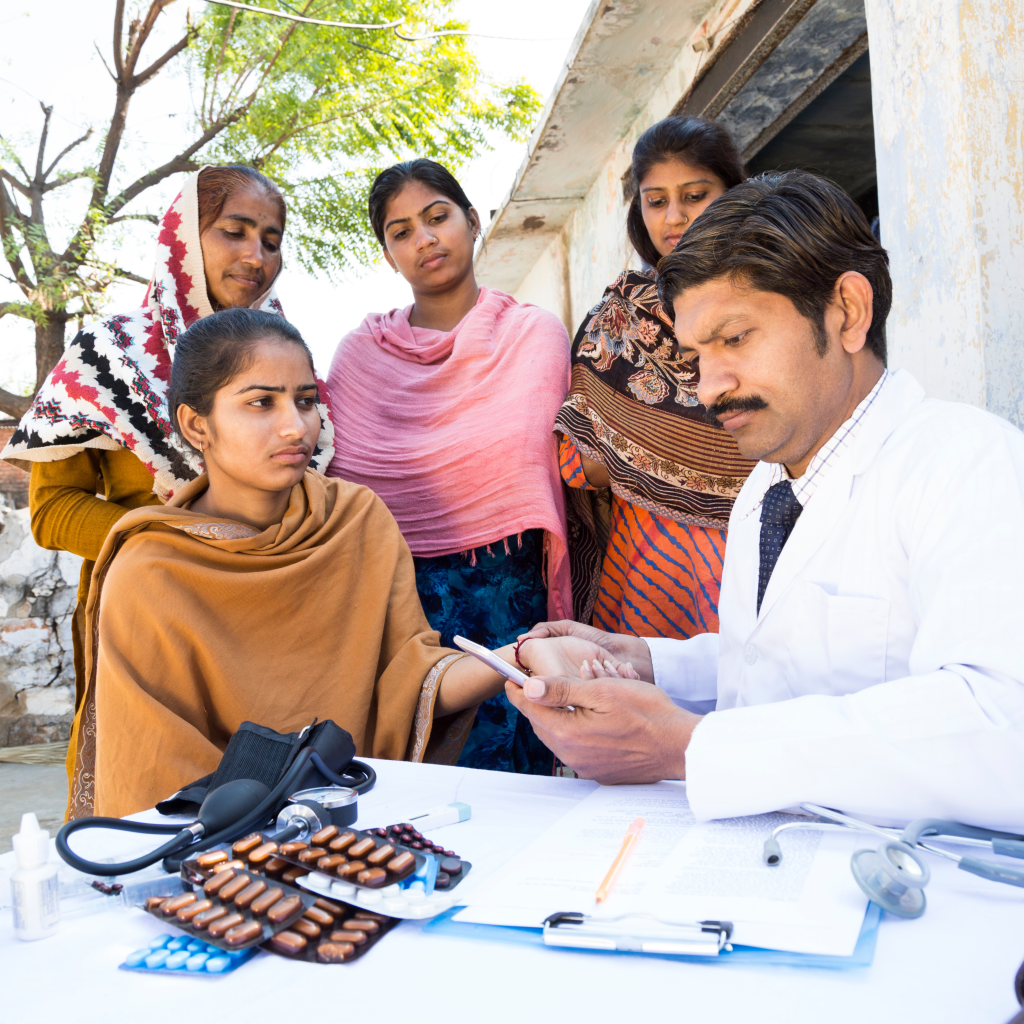
Limited healthcare access in Uttar Pradesh directly contributes to a decline in overall health outcomes, particularly in areas such as malnutrition, infectious diseases, and diagnostic capabilities.
- Malnutrition: Inadequate healthcare access exacerbates malnutrition rates. Without proper antenatal care, exclusive breastfeeding, and complementary feeding practices, children are more likely to suffer from stunting, wasting, and undernutrition. For instance, Uttar Pradesh has one of the highest rates of stunting in India, with nearly 38.4% of children under five affected. (Source: National Family Health Survey, NFHS-5)
- Infectious Diseases: A lack of access to preventive care, early diagnosis, and treatment fuels the spread of infectious diseases. Diseases like malaria, tuberculosis, and diarrhea thrive in these conditions. Uttar Pradesh contributes to a significant portion of India’s malaria burden, with certain districts reporting incidence rates as high as 10 cases per 1,000 population. (Source: National Vector Borne Disease Control Program)
- Diagnostic Challenges: Limited access to diagnostic facilities and trained healthcare professionals hinders early detection of diseases, leading to delayed treatment and increased morbidity. This is particularly evident in non-communicable diseases, such as diabetes and hypertension, where early diagnosis is crucial for effective management. It is estimated that only 30% of the population in rural India has access to basic diagnostic services. (Source: National Health Profile)
Limited Healthcare Access: A Draining Economic Burden
Limited healthcare access in Uttar Pradesh imposes a substantial economic burden on both individuals and the state.
Individual Burden

- Out-of-pocket health expenditures can be catastrophic for many families. A study by the National Sample Survey Office found that 42% of rural households in India incurred catastrophic health expenditures, meaning they spent more than 10% of their annual consumption on healthcare. (Source: National Sample Survey Office)
- Illness and disability often lead to lost income. In India, it’s estimated that out-of-pocket health payments contribute significantly to poverty and can trap families in a cycle of deprivation. (Source: World Bank)
- To cover medical costs, families may resort to selling assets or withdrawing children from school. This has a ripple effect on the overall well-being of the household.
Societal Burden
- The economic burden of ill health is substantial for the state. A significant portion of public health expenditure is directed towards treating preventable diseases, diverting funds from other essential sectors.
- Low health status can hinder economic growth and development. A study by the World Bank found that improved health can lead to significant economic gains. (Source: World Bank)
- The disproportionate impact of ill health on women can limit their economic participation and contribute to gender inequality.
Limited Healthcare Access: A Cycle of Poverty and Deprivation
Limited healthcare access in Uttar Pradesh has profound social implications, perpetuating a cycle of poverty and deprivation.
- Education Disruptions: Ill health among children often leads to absenteeism and dropout rates, hindering educational attainment. A study by UNICEF found that children from households without access to healthcare are 20% more likely to be out of school compared to their peers with better access. (Source: UNICEF)
- Reduced Productivity: Poor health reduces an individual’s ability to work and contribute to the economy. This can lead to lower incomes, decreased savings, and limited opportunities for social and economic mobility. It is estimated that illness and disability contribute to a 5% loss in GDP in developing countries. (Source: World Bank)
- Social Isolation: Chronic illnesses and disabilities can lead to social isolation and stigma. Individuals may withdraw from social activities and face discrimination, further exacerbating their challenges.
- Intergenerational Poverty: The impact of poor health can be intergenerational, with children from unhealthy families facing a higher risk of poor health, malnutrition, and limited educational opportunities. Children born into poverty are twice as likely to remain in poverty as those from wealthier families if they do not have access to basic healthcare services. (Source: World Bank)





